Abstract
Context: Allogeneic hematopoietic stem cell transplant (HCT) represents a curative option in acute myeloid leukemia (AML) in patients older then 60 years. The use of reduced intensity conditioning regimens (RIC) has decreased treatment related toxicity and minimized the role of age as a limiting factor. Other variables such as disease status, cytogenetics, donor type and comorbidities gained importance in the pre-transplant risk assessment. In 2014, Sorror et al., proposed a risk-adapted strategy, integrating AML-, HCT- and patient-specific risk factors to guide decisions about HCT versus no HCT in elderly patients.
End points: To determine overall survival (OS; defined as time to death irrespective of the cause), Relapse-free survival (RFS; defined as survival without death or relapse), non-relapse mortality (NRM; defined as time to death without evidence of disease relapse) and cumulative incidence of relapse (RI; defined as time to relapse). To evaluate, after stratifying patients according to the risk-adapted treatment strategy, the NRM rate, relapse rate and survival rate according to the HCT-CI comorbidity score.
Study design: We analyzed retrospectively, between 2010 and 2016, a cohort of AML patients, aged 60 years or older, treated and followed in our center. We classified the patients according to the risk-adapted strategy into 3 categories: favorable, intermediate and unfavorable risk.
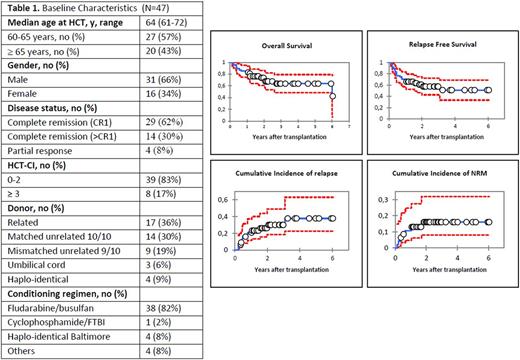
Results: 47 patients were included. The median age was 64 years (range 61-72). 29 (62%) patients were transplanted in first complete remission. All patients received a RIC. Patients and transplant characteristics are summarized in table 1. With a median follow-up of 6 years (range 1.5 month-6 years), OS at 1 and 3 years were respectively 83% (95% CI: 72-94%) and 63% (95% CI: 48-79%). The RFS at 1 and 3 years were 68% (95% CI: 55-81%) and 57% (95% CI: 42-72%) respectively. The cumulative incidence of relapse at 1 and 3 years were 20% (95% CI: 12-37%) and 30% (95% CI: 18-49%) respectively. The cumulative incidence of NRM at 1 and 3 years were 13% (95% CI: 6-27%) and 16% (95% CI: 8-31%). There was no significant difference in terms of OS, RFS and NRM for the type of donor and type of conditioning regimen.
Using the risk-adapted strategy, two patients had a favorable risk, 17 patients an intermediate risk and 28 patients an unfavorable risk. In the intermediate risk group, all patients had a low HCT-CI (score 0-2) comorbidity score. The NRM rate was 25% (4 patients). 75% (13 patients) were still alive and free from disease.
In the unfavorable risk group, 20 patients had a low and 8 patients a high (score>3) HCT-CI. In patients with a low HCT-CI, the relapse and NRM rates were 21% (n=6) and 7% (n=2) respectively and 43% (n= 12) were still alive at the last follow-up. In patients with a high HCT-CI, the relapse and NRM rate were 4% (n=1) and 11% (n=3) respectively and 14% (n=4) were still alive at the last follow-up.
Conclusion: Our study shows a low transplant-related toxicity with promising long-term outcome in patients aged 60 years or more. The observed RFS and OS, especially in the unfavorable risk AML patients, compare favorably with the results obtained with chemotherapy alone and suggest this population benefits from allogeneic HCT regardless of the HCT-CI comorbidity score. However, longer follow-up and further randomized trials are still needed.
De Botton: Servier: Honoraria; Pfizer: Honoraria; Novartis: Honoraria; Celgene: Honoraria; Agios: Honoraria, Research Funding. Ribbag: Servier: Consultancy, Honoraria; ArgenX: Research Funding; Roche: Honoraria, Other: travel, accommodation, expenses; BMS: Consultancy, Honoraria; MSD: Consultancy, Honoraria; Infinity: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; Nanostring: Consultancy, Honoraria; Epizyme: Consultancy, Honoraria; Pharmamar: Consultancy; Esai: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.